Diuretics
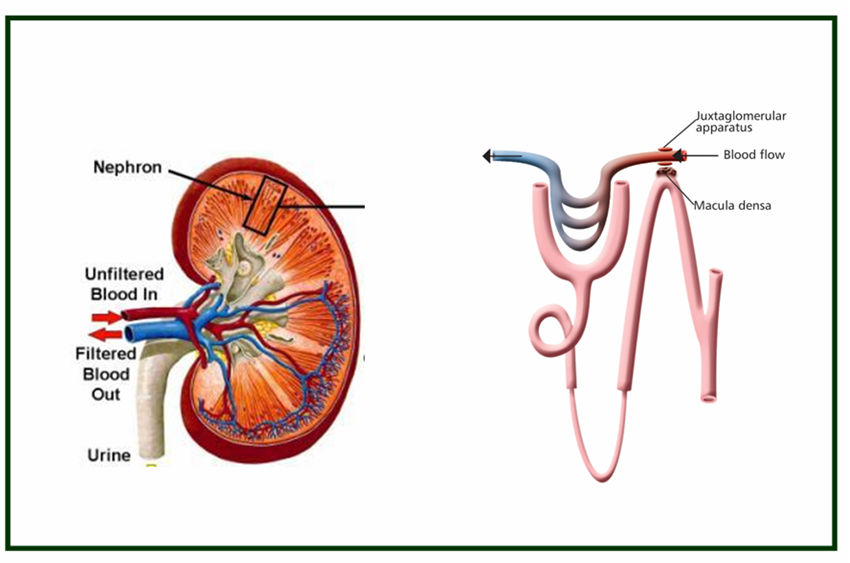
Diuretic agents are drugs that increase renal excretion of water and solutes. These are the drugs that are used to reduce the abnormal accumulation of excess fluid in the body. These diuretics can do this by eliminating the excess fluid through increasing the volume of urine excretion.
Side effect of diuretics: Hypercalcemia, hypokalemia, acidosis, metabolic alkalosis and hyponatremia.
|
Type |
Example |
Site of action |
Mechanism
|
|
Carbonic anhydrase (CA) |
Acetazolamide |
Proximal tubule |
inhibition of CA
|
|
Osmotic diuretics |
Mannitol |
Loop of Henle (DTL) |
Osmotic action Proximal tubule |
|
Loop diuretics |
Furosemide |
Loop of Henle |
inhibition of Na+-K+- 2Cl- symport |
|
Thiazide |
Hydrochlorothiazide |
Distal convoluted |
inhibition of Na+ Cl tubule symport |
|
Potassium-sparing diuretics (1) Na+ channel (2)Aldosterone antagonist |
Triamterene
Spironolactone |
Cortical collecting tubule
|
inhibition of Na+ channel inhibition of aldosterone receptors
|
Carbonic anhydrase (CA) inhibitors: Dichlorphenamide, acetazolamide
Mechanism of action: This class of diuretics inhibits carbonic anhydrase in the membrane and cytoplasm of the epithelial cells. The primary site of action is in proximal tubules. In the proximal tubule, Na+-H+ anti-port in the apical membrane of epithelial cells transports H+ into tubular lumen in exchange for Na+ movement into the cytoplasm. Na+ in the cytoplasm is pumped out to the inter-stitium by sodium pump. H+ in the lumen reacts with HCO3- to form H2CO3. H2CO3 is dehydrated to CO2 and H2O. This reaction is catalyzed by carbonic anhydrase in the luminal membrane. Both CO2 and H2O can permeate into cells, and rehydrate to form H2CO3. The rehydration is catalyzed by the cytoplasmic carbonic anhydrase. H2CO3 dissociates to form H+ which is secreted into lumen, and HCO3- which is transported into interstitium. Inhibition of anhydrase thus inhibits HCO3- reabsorption. Accumulation of HCO3- in the tubular lumen subsequently inhibits Na+-H+ exchange and Na+ reabsorption. The increase in sodium concentration in the tubular fluid may be compensated partially by increased NaCl reabsorption in later segments of the tubule. Thus, the diuretic effect of the carbonic anhydrase inhibitors is mild.
Clinical indications: Treatment of cystinuria, Glaucoma, Metabolic alkalosis and acute mountain sickness.
Side effects: Renal stones, drowsiness, rash, fever and interstitial nephritis.
Osmotic diuretics: Urea, glycerin, mannitol, isosorbide
Mechanism of action: The primary sites of action for osmotic diuretics are the Loop of Henle and the proximal tubule where the membrane is most permeable to water. These are the substances to which the tubule epithelial cell membrane has limited permeability. Osmotic diuretics significantly increase the osmolarity of plasma and tubular fluid when administered (often in a large dosage). The osmotic force thus generated prevents water reabsorption and also extracts water from the intracellular compartment, expands extracellular fluid volume and increases renal blood flow resulting in reduced medulla tonicity.
Clinical indications:
Side effects: Dehydration, hypernatremia, nausea, headache, and vomiting. In patients with congestive heart failure, expansion of extracellular volume may produce pulmonary edema.
Loop diuretics: Furosemide, ethacrynic acid, bemetanide, torsemide.
Loop diuretics are highly efficacious and thus are called as high ceiling diuretics.
Mechanism of action: Loop diuretics inhibit reabsorption of NaCl and KCl by inhibiting the Na+-K+-2Cl- symport in the luminal membrane of the thick ascending limb (TAL) of loop of Henle. As TAL is responsible for the reabsorption of 35% of filtered sodium, and there are no significant downstream compensatory reabsorption mechanisms. As the Na+-K+-2Cl- symport and sodium pump together generate a positive lumen potential that drives the reabsorption of Ca++ and Mg++, inhibitors of the Na+-K+-2Cl- symport also inhibit reabsorption of Ca++ and Mg++.
Clinical indications: Pulmonary edema, Hypercalcemia.
Side effects: Ototoxicity, Hypokalemic metabolic alkalosis, Hypomagnesaemia, Allergic reactions and Hyperuricemia.
Thiazide diuretics: Chlorothiazide, Hydrochlorothiazide, Chlothalidone, Indapamide Metolazone, Quinethazone.
Mechanism of action: These drugs inhibit a Na+-Cl- symport in the luminal membrane of the epithelial cells in the distal convoluted tubule. Thus, Thiazide inhibits NaCl reabsorption in the distal convoluted tubule, and may have a small effect on the NaCl reabsorption in the proximal tubule. Thiazides enhance Ca++ reabsorption in the distal convoluted tubule by inhibiting Na+ entry and thus enhancing the activity of Na+-Ca++ exchanger in the basolateral membrane of epithelial cells.
Clinical indications: Hypertension, Nephrolithiasis due to hypercalciuria, Edema associated with congestive heart failure, hepatic cirrhosis and renal diseases, Nephrogenic diabetes insipidus.
Side effects: Hypotension, alkalosis, hyperuricemia, hypochloremia and hypomagnesaemia.
Potassium-sparing diuretics:
Mechanism of action: Amiloride and triamterene inhibit the sodium channel in the luminal membrane of the collecting tubule and collecting duct. This sodium channel is critical for Na+ entry into cells down the electrochemical gradient created by sodium pump in the basolateral membrane, which pumps Na+ into interstitium. This selective trans-epithelial transport of Na+ establishes a luminal negative trans-epithelial potential which in turn drives secretion of K+ into the tubule fluid. The luminal negative potential also facilitates H+ secretion via the proton pump in the intercalated epithelial cells in collecting tubule and collecting duct. Inhibition of the sodium channel thus not only inhibits Na+ reabsorption but also inhibits secretion of K+ and H+, resulting in conservation of K+ and H+.
Clinical indication: Liddle's syndrome
Side effects: nausea, vomiting, headache, hyperkalemia.
Aldosterone antagonists: Spironolactone competitively inhibits the binding of aldosterone to its receptor and abolishes its biological effects. Aldosterone, by binding to its receptor in the cytoplasm of epithelial cells in collecting tubule and duct, increases expression and function of Na+ channel and sodium pump, and thus enhances sodium reabsorption.
Clinical indication: Edema
Side effects: Gynecomastia, impotence and hirsutism.
Diuretics, thiazides, mannitol