Sedatives: These are the drugs which reduce excitement without producing sleep.
Hypnotics: Drugs which produce sleep resembling natural sleep.
Sedative-Hypnotic
Sedative: A substance that induces sedation by reducing irritability and excitement.
Hypnotic: A drug which induces a state of drowsiness.
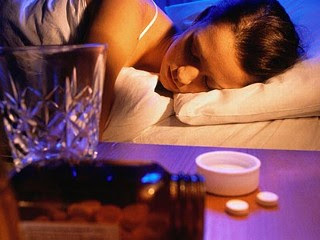
Sedative-hypnotics are drugs which depress or slow down the body’s functions. Often these drugs are referred to as tranquilizers and sleeping pills or sometimes just as sedatives. Their effects range from calming down anxious people to promoting sleep. Both tranquilizers and sleeping pills can have either effect, depending on how much is taken. At high doses or when they are abused, many of these drugs can even cause unconsciousness and death.
Treatment:
Benzodiazepines: Diazepam, midazolam, alprazolam and triazolam
Benzodiazepines exert their effect by selectively binding to GABAA receptors and enhancing its inhibitory effect on the CNS. GABA receptor contains more than one isoform each with different subunits:
1. α1-subunit→ sedation, amnesia and possibly antiseizure effects.
2. α 2 -subunit → anxiolytic and muscle relaxing action.
3. α5-subunit→ memory impairment.
Benzodiazepines bind to many isoforms of the GABA receptor at different areas of the brain. The GABA receptor is a pentameric receptor consisting from five subunits in variant isoforms. The major isoform is composed of five subunits comprising of 2α, 2β, and one γ subunits.
Pharmacokinetics: The rate of oral absorption varies depending on each drug’s lipophilicity. Diazepam and the active metabolite of clorazepate have more rapid absorption than other benzodiazepines. Absorption of triazolam is extremely rapid. Benzodiazepines bind strongly to plasma proteins. They also accumulate in body fats with high volume of distribution. Benzodiazepines are metabolized by oxidation and hydroxylation by cytochrome P450 especially isoform CYP3A4 (phase I). The metabolites are subsequently conjugated (phase II) to form glucuronides that are excreted in the urine. All sedative-hypnotics cross the placental barrier during pregnancy. They are also detectable in breast milk. The metabolism of diazepam, midazolam, and triazolam is affected by inhibitors and inducers of hepatic P450 isozymes.
Side effects: Drowsiness, confusion, amnesia, decrease in motor coordination, and decrease in psychomotor performances.
Pharmacological Effects: Reduction of anxiety & aggression, Sedation, Hypnotic.
Barbiturates: Phenobarbitone, mephobarbitone, secobarbitone, pentobarbitone, thiopentone, hexobarbitone.
Barbiturates are able to enhance the action of GABA by prolonging the duration of chloride channel opening. At high doses, barbiturates can actually act directly on GABA’s receptor. They have a depressant effect similar to general anesthetics due to their broad inhibitory effect on various CNS receptors.
Pharmacokinetics: Barbiturates are absorbed rapidly into the blood following their oral administration. Their metabolic pathway involves oxidation by hepatic enzymes to form substances which appear in the urine as glucuronide conjugates. Phenobarbital is the only barbiturate excreted unchanged in the urine (20–30%), and its elimination rate can be increased significantly by alkalinization of the urine where it is considered a weak acid.
Adverse Effects: Barbiturates induce the hepatic cytochrome P450 inducing increased metabolic degradation. Barbiturates, in relation to benzodiazepines, are more likely to causes cardiovascular and respiratory depression. Also, barbiturates do aggravate porphyria crisis.
Zolpidem: The hypnotic zolpidem is not a benzodiazepine in structure, but it acts on a subset of the benzodiazepine receptor. Zolpidem has no anticonvulsant or muscle-relaxing properties. It
Shows little withdrawal affects, and exhibits minimal rebound insomnia, and little or no tolerance occurs with prolonged use. Zolpidem is rapidly absorbed from the gastrointestinal tract, and it has a rapid onset of action and short elimination half-life. Zolpidem undergoes hepatic oxidation by the cytochrome P450 system to inactive products.
Adverse effects: Agitation, nightmares, headache, gastrointestinal upset, dizziness, and daytime drowsiness.
Zaleplon: Zaleplon causes fewer residual effects on psychomotor and cognitive functions compared to zolpidem or the benzodiazepines. This may be due to its rapid elimination, with a half-life that approximately 1 hour. The drug is metabolized by CYP3A4.
Eszopiclone: Eszopiclone is an oral non-benzodiazepine hypnotic and is also used for treating insomnia. Eszopiclone is rapidly absorbed, extensively metabolized by oxidation and demethylation via the cytochrome enzyme system and mainly excreted in the urine. Elimination half-life is approximately 6 hours.
Adverse effects: Dry mouth, anxiety, headache, peripheral edema, somnolence, and unpleasant taste.
Ramelteon: It is a selective agonist at the MT1 and MT2 subtypes of melatonin receptors. Normally, light stimulating the retina transmits a signal to the supra chiasmatic nucleus (SCN) of the hypothalamus, that in turn relays a signal via a lengthy nerve pathway to the pineal gland that inhibits the release of melatonin from the gland.
Adverse effects: Fatigue, dizziness, and somnolence.
Chloral hydrate: Chloral hydrate is a trichlorinated derivative of acetaldehyde that is converted to the active metabolite trichloroethanol in the body. The drug is an effective sedative and hypnotic that induces sleep in about 30 minutes and the duration of sleep is about 6 hours. Chloral hydrate is irritating to the gastrointestinal tract and causes epigastric distress. It also produces an unusual, unpleasant taste sensation. It synergizes with ethanol.
Antihistamines: Nonprescription antihistamines with sedating properties, such as diphenhydramine and doxylamine, are effective in treating mild types of insomnia. However, these drugs are usually ineffective for all but the milder forms of situational insomnia.
Ethanol: Ethyl alcohol (Ethanol) has anxiolytic and sedative effects, but its toxic potential outweighs its benefits. Alcoholism is a serious medical and social problem. Ethanol is a CNS depressant, producing sedation and, ultimately, hypnosis with increasing dosage. It is readily absorbed orally and has a volume of distribution close to that of total body water. Ethanol is metabolized primarily in the liver, first to acetaldehyde by alcohol dehydrogenase and then to acetate by aldehyde dehydrogenase. Elimination is mostly through the kidney, but a fraction is excreted through the lungs.
Disulfiram: Disulfiram blocks the oxidation of acetaldehyde to acetic acid by inhibiting aldehyde dehydrogenase. This results in the accumulation of acetaldehyde in the blood, causing flushing, tachycardia, hyperventilation, and nausea.
Naltrexone: It is a long-acting opiate antagonist. It is better tolerated than disulfiram and does not produce the aversive reaction that disulfiram does.
Sedation, barbiturates, benzodiazepines